Genetic carrier screening began in the 1970s with the expectation of identifying couples at-risk for genetic disorders of childhood onset. Screening was practical only within ethnic groups in which prevalence of a specific autosomal recessive disorder was high. Initially, this included Tay-Sachs disease in Ashkenazi Jewish individuals, sickle cell anemia in Africans and African-Americans, and B-thalassemia in multiple ethnic groups but especially Italians, Greeks, and Turks. Only a limited number of disorders could be screened because protein-based (gene product) assays were the only methodology capable of distinguishing carriers (heterozygotes) from homozygous normal individuals. Not until 2001 could a common genetic disorder (cystic fibrosis) be screened solely by DNA-based platforms. Screening is now pan-ethnic, and uses DNA platforms. Couples of mixed ethnicities are screened without regard to specific ethnicity. Over 400 disorders can be screened, identifying approximately 2% at-risk couples.
Expanded pan-ethnic carrier screening panels mostly identify at-risk couples for homozygous autosomal recessive childhood-onset conditions. However, these same platforms also identify adults who are heterozygous (carriers) not only for carriers for a childhood condition, but clinically at-risk for their own separate adult-onset disorder. Illustrative examples include Fanconi anemia (FAN) and ataxia telangiectasia (ATM). These autosomal recessive childhood-onset conditions are caused by defects in DNA repair. Parents of an affected child would be expected to be asymptomatic carriers based only their child’s phenotype. If only a single parent were heterozygous, ordinarily no further action would be sought nor information possible. However, with DNA- based screening, heterozygous women could be identified. That is, heterozygous women for FAN or ATM are at-risk themselves for developing adult-onset breast cancer.
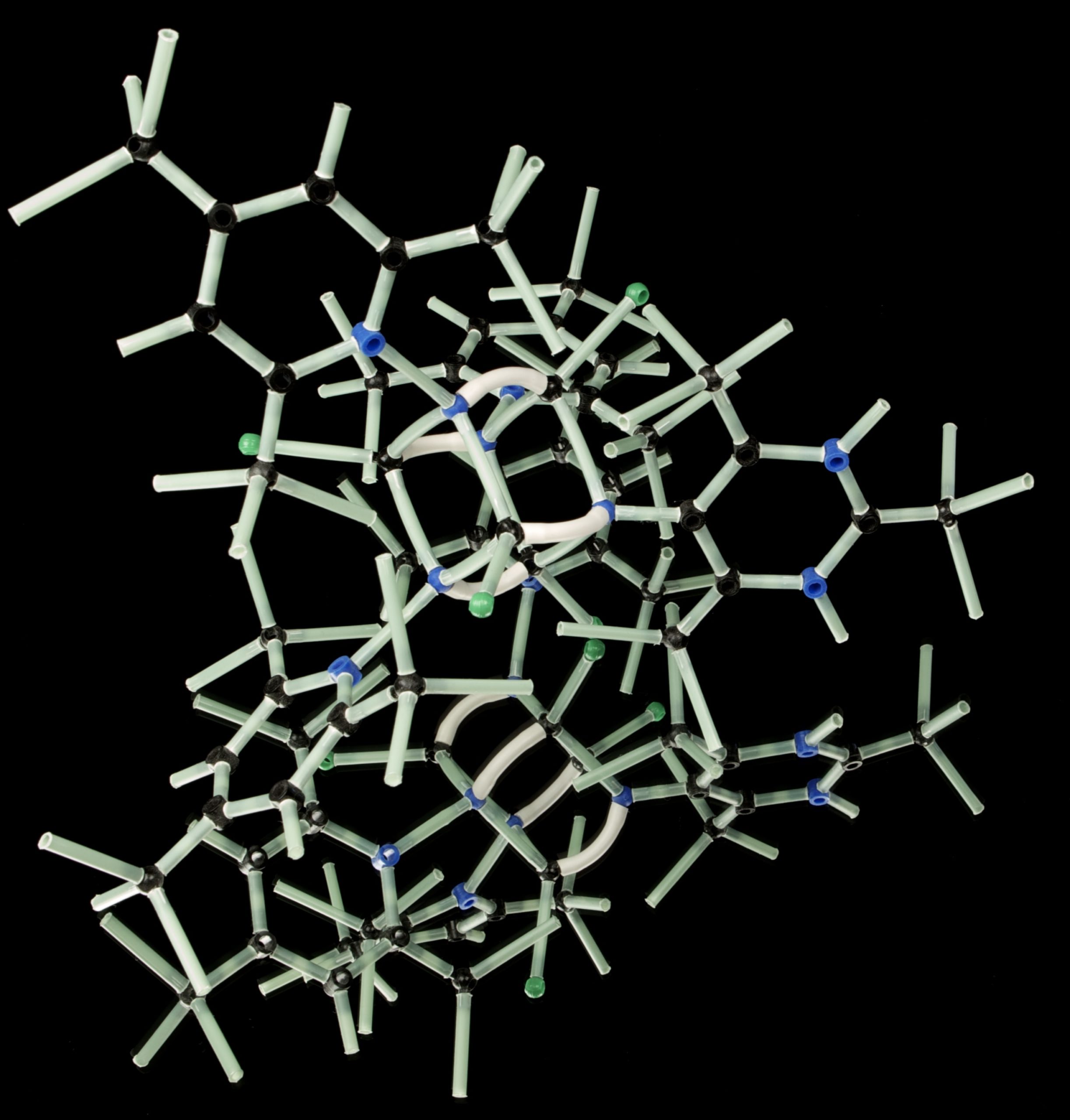
Adult women with breast cancer may have also undergone gene panel testing to determine whether they have mutations in one of the many cancer-susceptibility genes. The NIH National Cancer Institute (NCI) tabulates 31 Familial Cancer Susceptibility Syndromes (https://www.cancer.gov/about-cancer/causes-prevention/genetics/overview-pdq). Typically most are adult-onset and autosomal dominant. At Reproductive Genetic Innovations, over 800 cancers have been studied through Preimplantation Genetic Testing (PGT). These cases were often ascertained after another family member (for example the mother) learned she/he had cancer due to a heritable mutation. Although she would typically be beyond reproductive age, her offspring and grandchildren would not. A clinically normal son or daughter of a mother with an autosomal dominant breast cancer soon realized they could have the same cancer-susceptibility gene and could transmit the pathogenic (disease-causing) variant to their own offspring. These children could avoid transmission by monitoring the pregnancy through chorionic villus sampling (CVS) or amniocentesis; however, there would exist a 50% likelihood of needing clinical pregnancy termination to avoid an affected liveborn. Instead, an embryo could be selected and transferred to avoid offspring having the familial pathogenic variant. At Reproductive Genetic Innovations, selecting an embryo without the cancer susceptibility variant has increased two-fold since 2015. Preimplantation genetic testing requires an In Vitro Fertilization (IVF) cycle, but couples who wish to avoid transmission of a previously identified cancer-susceptibility gene mutation choose PGT-M (Preimplantation Genetic Testing for a Monogenic or Single Gene defect) in more than half the cases.
The parent with a transmissible cancer susceptibility gene could be either female or male. Over a 70-year lifespan, risks to women with BRCA1 or BRCA-2 are 87% for breast cancer and 63% for ovarian cancer. For males risks are 20% for prostate cancer and 7% for pancreatic cancer.
PGT for adult-onset cancer susceptibility is straight forward and accurate. However, diagnostic complexity due to molecular heterogeneity in adult onset disorders must be taken into account. The precise DNA change responsible for a given adult-onset cancer must be determined, and many different pathogenic varinats are responsible. Among cases having a BRCA1 pathogenic variants that have been managed at Reproductive Genetic Innovations, 51% were due to a DNA mutation at a single predominant site in that gene, namely deletion of adenine and guanine at codon 187 (187delAG). The other 49% of BRCA1 cases were comprised of 37 different mutations found in only a single family and 5 found in no more than 3 families. In BRCA2, the same patterns were seen. Deletion of thymine at codon 6174 accounted for 40% of mutations, but the 29 different mutations responsible for the remaining 60% were each present in only a single family. The diagnostic significance is that performing PGT for adult onset disorders cannot be based on testing a limited number of the most common causative pathogenic variants. Only a relatively small proportion of cases would be detected, with many false negative results.
Adult onset PGT-M is utilized at RGI for other adult-onset autosomal dominant conditions. The most common cardiac disorders are autosomal dominant Long Q-T syndrome; hypertrophic cardiomyopathy; and dilated cardiomyopathy. These mutations are not infrequently ascertained in the context of physical exertion by young athletes. Analogous to cancer susceptibility genes, family members learn the genetic basis of their relative with such a cardiac disorder, wish to avoid transmission of the causative gene to their own offspring, and undergo PGT-M for embryo selection. Similar circumstances arise in heritable neurodegenerative disorders. Common neurodegenerative disorders in which embryo selection is chosen include Huntington disease and early onset (<50 years) Alzheimer’s disease.
By: Joe Leigh Simpson, MD, FACMG, FACOG, FRCOG – Clinical Director

Leave a Reply